Salmonella Infection: Causes, Symptoms and Control

This post is also available in:
This post is also available in:
![]() Español (Spanish)
Español (Spanish) ![]() हिन्दी (Hindi)
हिन्दी (Hindi) ![]() Ελληνικά (Greek)
Ελληνικά (Greek)
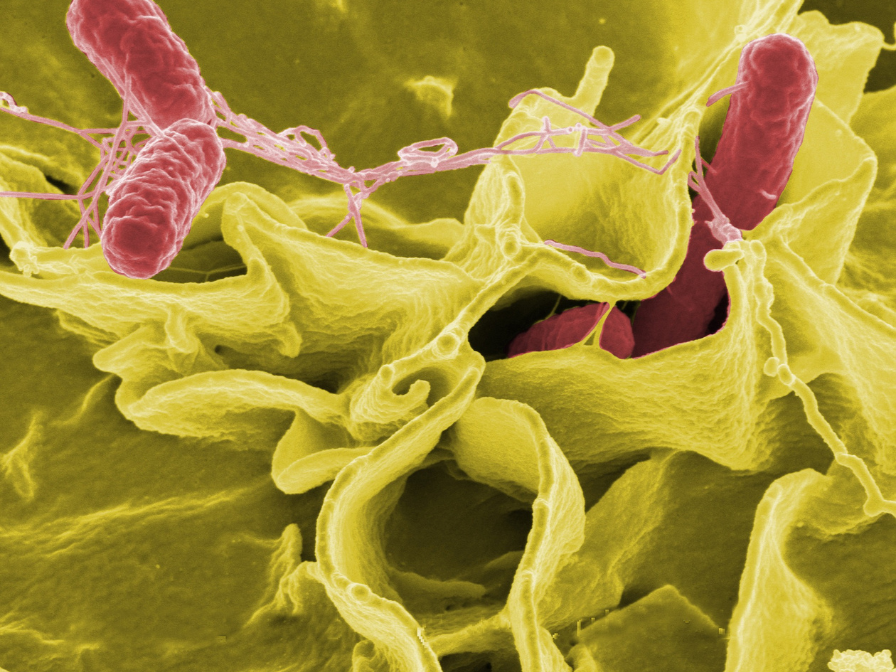
Microbial Overview
What are the main types of Salmonella?
Salmonella is a genus of a gram-negative, rod-shaped motile bacteria. It belongs to the Enterobacteriaceae family. Most types of Salmonella cause salmonellosis (foodborne illness), while some other types of Salmonella cause typhoid fever or paratyphoid fever.
The most common species of Salmonella are:
- Salmonella enterica and
- Salmonella bongori
Salmonella enterica is divided into six strains. Each strain has distinct genetic and antigenic characteristics, which contribute to differences in their pathogenicity, host range, and disease manifestations.
What are the different strains of Salmonella?
Salmonella Typhimurium: This strain is one of the most prevalent causes of salmonellosis worldwide. It can infect a broad range of hosts, including humans, livestock, and pets and is associated with gastroenteritis in humans and animals.
Salmonella Enteritidis: S. Enteritidis is another significant cause of salmonellosis, particularly associated with contaminated eggs and poultry products. It is known for causing gastrointestinal illness in humans.
Salmonella Typhi: Unlike many other Salmonella strains, which primarily cause self-limiting gastroenteritis, S. Typhi is responsible for typhoid fever. It is transmitted through contaminated food or water and can lead to a severe infection. Typhoid fever is a more serious condition that requires medical attention.
Salmonella Paratyphi: Similar to S. Typhi, S. Paratyphi causes a systemic infection known as paratyphoid fever. It is less severe than typhoid fever but shares similar symptoms. Both S. Typhi and S. Paratyphi are associated with human-to-human transmission.
What toxins does Salmonella produce?
Salmonella produces endotoxins and exotoxins. The exotoxins of Salmonella are divided into:
- enterotoxins and
- cytotoxins
Endotoxins: Salmonella bacteria have endotoxins on their outer membrane. When the bacteria are destroyed or broken apart, these endotoxins are released. Endotoxins can trigger an inflammatory response in the body and contribute to the symptoms of salmonellosis.
Enterotoxins: Salmonella can produce enterotoxins that affect the small intestine. These toxins disrupt the normal function of the intestinal cells, leading to increased secretion of water and electrolytes into the intestines.
Cytotoxins: Some strains of Salmonella produce cytotoxins that can damage host cells. These toxins can cause cell death or impair cellular function, contributing to tissue damage and inflammation.
It’s important to note that the clinical picture and severity of the illness can vary among different Salmonella strains, and certain strains may be more prevalent in specific geographical regions or associated with particular food sources.
In which conditions is Salmonella resistant?
- Oxygen requirements: facultative anaerobe
- Temperature range for growth: 5-47 ºC
- pH range for growth: 3.5 – 9.6
- Water activity: 0.9 – 0.95 minimum
- Non-spore-forming
- Heat sensitive
- Survives in refrigerated, frozen, or dehydrated foods for long periods
What is the incidence and prevalence of Salmonella?
According to Baiyan Cong et al., 2002; non-typhoidal Salmonella is a common cause of bacterial enteritis in humans, causing 93.8 million cases and 155,000 gastroenteritis deaths globally every year.
In the European Union, there are over 91,000 reported cases of salmonellosis annually in humans, accounting for a rate of 20 cases per 100,000 individuals. According to data from the European Food Safety Authority (EFSA), it is estimated that the economic burden of salmonellosis worldwide amounts to approximately €3 billion per year.
In US, CDC estimates Salmonella bacteria cause about 1.35 million infections, 26,500 hospitalizations, and 420 deaths annually.
Which population groups are at higher risk of being infected by Salmonella?
Everyone who consumes contaminated food or water is at risk. However, the population groups susceptible to Salmonella infections are:
- Children under the age of 5.
- Infants and adults aged 65 and older.
- People with a weakened immune system
- People taking certain medicines (for example, stomach acid reducers)
Where is Salmonella most commonly found?
Salmonella infections can be contracted from a wide range of food sources, including (undercooked) poultry, beef, pork, eggs, milk, fruits, sprouts, various vegetables, as well as processed foods like nut butter, raw egg desserts, mayonnaise, frozen pot pies, flour, peanut butter, dried milk products, chocolates, prepackaged salads and others.
Apart from the food sources, people can get Salmonella infection from contaminated water and by touching infected animals, their feces, or their environment.
It is important to note that contaminated foods usually look and smell normal, but it is not safe to eat them.
What are the symptoms of Salmonella?
Non-typhoidal Salmonella
Regarding non-typhoidal Salmonella, typically symptoms appear within 6 to 72 hours after exposure. The symptoms can last up to 7 days, they vary in severity and may include the following: Diarrhea, abdominal cramps, fever, nausea and vomiting, headaches, muscle pain or blood in the stool, rarely leading to bacteremia or meningitis.
Typhoidal Salmonella
Typhoidal Salmonella refers to a specific group of Salmonella serotypes that cause systemic illness in humans, leading to a severe life-threatening condition known as typhoid fever (enteric fever). These serotypes include Salmonella Typhi and Salmonella Paratyphi. The clinical picture of typhoid fever includes fever, headache, anorexia, malaise, myalgias and sometimes cough. The symptoms appear after an incubation period of 10 to 14 days. It is more common in developing countries.
How long does it take to get over Salmonella?
For most people, the symptoms will last for 5 to 7 days. However, depending on the strain and the severity, it is possible to last longer.
How is Salmonella transmitted?
Transmission can occur through various routes. The main modes of transmission are:
- Foodborne
- Waterborne
- Person to person
- Animal contact
Salmonella can be introduced through people, clothing, footwear, vehicles, utensils, equipment, litter, pests, rodents, food, feed, wild birds or pets.
Non-typhoidal salmonellosis is a global illness that affects both humans and animals. Animals are the primary source of the bacteria, and the disease is typically transmitted through contaminated food. However, person-to-person transmission is also possible. On the other hand, the Salmonella strains responsible for Typhoid fever and other enteric fevers are primarily spread from one person to another through the fecal-oral route and do not have significant animal reservoirs.
Which is the treatment for Salmonella?
If you suspect you have a Salmonella infection or have concerns about your symptoms, it is recommended to consult a healthcare professional for proper diagnosis and guidance.
What should I know about antimicrobial resistance and Salmonella?
Antimicrobial resistance occurs when bacteria and fungi become resistant to the drugs meant to eliminate them, allowing them to survive and multiply. Salmonella is showing increasing resistance to important antibiotics, which can reduce treatment choices for severe infections. One effective approach to combat antimicrobial resistance is the responsible and appropriate use of antibiotics.
How to control and prevent Salmonella?
Regarding your facilities, you need specific prevention or control measures. The most important measures are appropriate hygienic practices, thorough cooking and refrigeration.
Below you can find different prevention and control measures depending on the facilities you are.
How to prevent and control Salmonella at a household level and retailers?
How to prevent and control Salmonella in feed and feed ingredients?
How to control Salmonella in poultry?
References
Alphons J.A.M. van Asten , Jaap E. van Dijk, Distribution of “classic” virulence factors among Salmonella spp., FEMS Immunology & Medical Microbiology, Volume 44, Issue 3, June 2005, Pages 251–259, https://doi.org/10.1016/j.femsim.2005.02.002
Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Foodborne, Waterborne, and Environmental Diseases (DFWED)
Ontario Ministry of Health, Ministry of Long-Term Care, Salmonellosis
Gong Baiyan, Li Hong, Feng Yulian, Zeng Shihan, Zhuo Zhenxu, Luo Jiajun, Chen Xiankai, Li Xiaoyan, 2022, Prevalence, Serotype Distribution and Antimicrobial Resistance of Non-Typhoidal Salmonella in Hospitalized Patients in Conghua District of Guangzhou, China, Frontiers in Cellular and Infection Microbiology, 12, DOI=10.3389/fcimb.2022.805384
Popa GL, Papa MI. Salmonella spp. infection – a continuous threat worldwide. Germs. 2021 Mar 15;11(1):88-96. doi: 10.18683/germs.2021.1244. PMID: 33898345; PMCID: PMC8057844.
Giannella RA. Salmonella. In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 21. Available from: https://www.ncbi.nlm.nih.gov/books/NBK8435/
F.T. Jones, 2011, A review of practical Salmonella control measures in animal feed, Journal of Applied Poultry Research, Volume 20, Issue 1, Pages 102-113, ISSN 1056-6171, https://doi.org/10.3382/japr.2010-00281.